- Home
- Ongecategoriseerd
- From plague to Coronavirus
From plague to Coronavirus. A very brief history of epidemics in Flanders and Belgium.
DETAILS
Used datasets:
Date:
Category:
Author: Isabelle Devos
The coronavirus has dominated our daily lives for several months now. It seems as if COVID-19 is the most widespread infectious disease on earth. Statements such as ‘nothing will be the same again’ or ‘there will be a pre- and a post-Corona era’ intimate the worst possible scenarios.
Counting nearly 300,000 deaths (as of 15th May 2020) the coronavirus is, however, not (yet) nearly as deadly as many other infectious diseases. Tuberculosis, AIDS and malaria, the three so-called ‘big killers’, claim millions of lives every year, mostly in the southern hemisphere. Even the plague itself, yes the plague, is still responsible for thousands of infections a year. In fact, the island of Madagascar suffered a serious plague epidemic as recently as 2017.
In Europe and North America, however, we have not only forgotten how to handle epidemics, many of us have also forgotten that up to 100 years ago infectious diseases were the most common cause of death. It is therefore high time to refresh our memory.
Epidemiological transition (nineteenth to twentieth centuries)
General public health has considerably improved in the northern hemisphere since the early nineteenth century. Life expectancy has more than doubled in the last 200 years. In Belgium, it rose from around 37 years in 1830 to 47 years in 1900, 65 years in 1950 and 81.5 years today. However, progress has been far from equally distributed. It was greater for children than for parents and also for women than for men. The decline in death rates went hand-in-hand with a radical shift in causes-of-death. Infectious diseases such as smallpox, cholera and tuberculosis gradually changed places with degenerative diseases such as cardiovascular diseases and cancer. In technical parlance, this is referred to as ‘the epidemiological transition’. Of the circa 110,000 Belgians who die every year today, more than half are the result of cardiovascular diseases (28%) or cancer (26%).
Research attributes three main causes to the mortality decline of infectious diseases. While in the first phase improvement in hygiene and sanitary conditions played the primary role, during the nineteenth century increasing living standards were responsible (such as more and better nutrition). Only since 1945 has medicine (antibiotics and vaccines, chemotherapy, surgery etc) played a greater role. That is hardly surprising seeing that it is only since the late nineteenth century that we have been aware that bacteria, viruses and parasites cause diseases (the so-called ‘bacteriological revolution’).
Besides a shift from low to higher life expectancy and from infectious to chronic diseases, death rates today also reveal a more stable pattern, even though at this moment in time COVID-19 gives precisely the opposite impression. The yearly crude mortality rate (the number of deaths per thousand inhabitants), a number subject to strong fluctuations in the past, in Belgium decreased from between 30 and 45 deaths in the early nineteenth century to a constant of around 10 deaths in the late twentieth century. Although tuberculosis was the main cause of death during the nineteenth century , epidemics were caused by other diseases. Belgium was ravaged by cholera seven times in 1832-33, 1848-49, 1854, 1859, 1866, 1883-85 and 1891-95. With around 43,400 victims, the epidemic of 1866 was the most severe; it hit young active people the hardest. Typhoid, smallpox and influenza also caused mortality crises in 1846-47, 1871 and 1918-19 respectively.
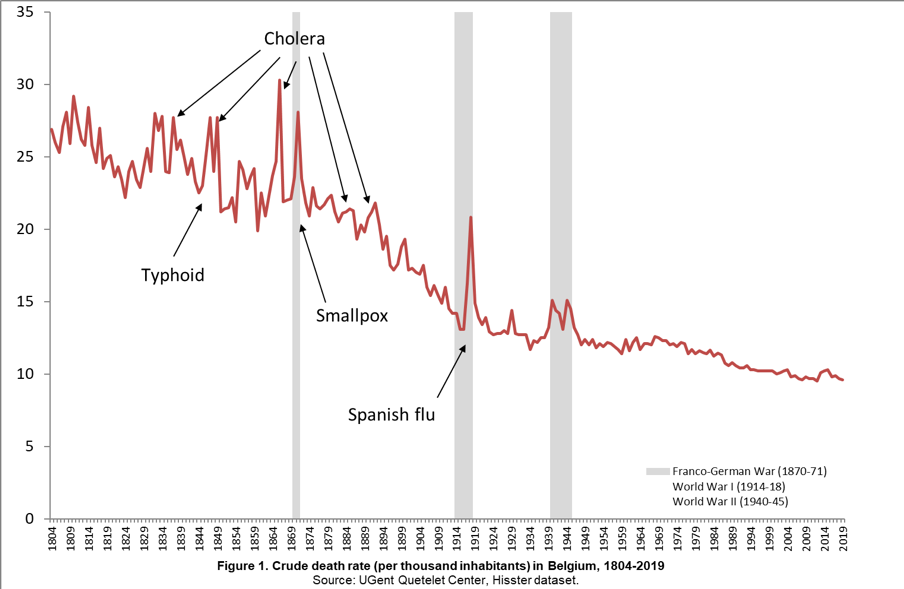
Such epidemics could display enormous regional variations. Hotspots of infection, as is the case today with COVID-19 in e.g. Limburg and Lombardy in Italy, are generally related to the place of the outbreak and the way in which the disease is transmitted, via people (tuberculosis, smallpox, COVID-19), via insects (malaria, the plague) or via water and food (cholera, typhoid, dysentery). In addition to population density and mobility, the social, economic and political context can also play an important role. As such, the typhoid epidemic of 1846-47 hit West- and East Flanders the hardest, regions which were both strongly affected by the crisis in the linen industry and in agriculture, while the cholera epidemic of 1866 mainly affected the larger cities, and the Spanish flu in 1918-19 was initially most deadly near the war front. The Spanish flu was also the last pandemic which Belgium was confronted by. Contemporaries estimated the death toll from the disease in Belgium to be around 20,000, however, based on data from the pandemic in neighbouring countries we can assume that the true number was at least double that.
Historical sources of excess mortality
The further one goes back in time the more difficult it is to identify the specific disease causing the outbreak of an epidemic. It was only after the cholera epidemic of the late 1840s that the specific cause of death was recorded for each case. Before this period, one has to interpret general descriptions given in medical accounts, chronicles and municipal records.
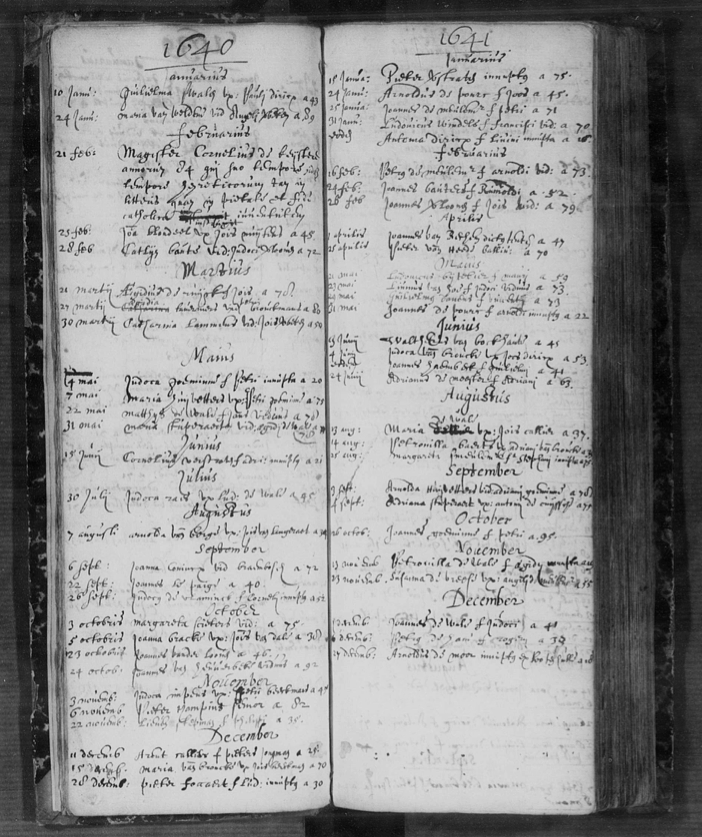
Furthermore, the calculation of the number of deaths and the spread of an epidemic also becomes more complex. The introduction of the civil register at the end of the eighteenth century meant every death was now recorded locally, however, this was not the case in previous centuries where one can only consult parish registers for notifications of burials and baptisms.
Just as there is a great deal of discussion today about the way in which excess mortality due to COVID-19 is recorded and calculated, much ink has also been spilt in historical research regarding the best indicator of excess mortality. Some authors will compare the number of deaths in the year of an epidemic with the average number of previous years. Others will consider the total number of the population and base their calculation on the crude mortality rate per thousand inhabitants.
In the absence of reliable population censuses in the Early Modern period (sixteenth to eighteenth centuries), such an indicator is not an option for the Southern Netherlands. An alternative is to calculate the ratio of the number of burials in relation to baptisms, a method that has already been used for Early Modern England. Depending on the indicator, the peaks in the graph can vary but at least the various methods usually do indicate excess mortality as occurring during the same years.
The Early Modern period (sixteenth to eighteenth centuries)
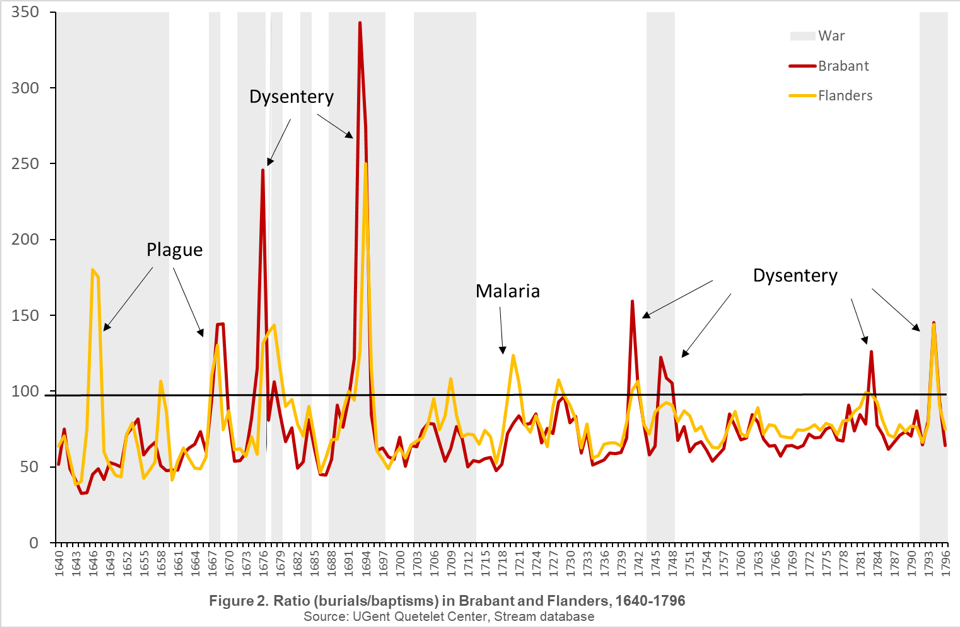
Using the large-scale STREAM database (UGent, Quetelet Center) we can map excess mortality in the Duchy of Brabant and the County of Flanders between 1640 and 1795. This comprises the yearly data of 507 parishes (out of a prior total of 1125). Ratios above 100 point to a greater number of burials than baptisms and a negative natural growth; ratios below 100 indicate a positive growth. Four peaks in the graph stand out: those at the end of both 1660 and 1670, and those in the middle of the years 1690 and 1790. During the eighteenth century, there were fewer peaks of excess mortality and, furthermore, these peaks were not as large.
During the eighteenth century, central government intervened to a greater extent at the level of public health and also started to take more preventative action. Before then public hygiene was left to local authorities. Each city and village approached this in their own particular way. Isolation and quarantine of (potentially) ill patients were the most commonly used measures.
In the Southern Netherlands, it was the battle against dysentery epidemics that constituted the hesitant beginnings of state intervention in such matters. As such, burying of the dead in churches and chapels was prohibited to counter stench and possible danger. Henceforth cities had to plan new burial grounds far away from church buildings and outside city walls.
From the middle of the nineteenth century on, sanitary measures were planned in conjunction with medical societies in a more structured way and with greater financial means. Infectious diseases were gradually pushed back when central and local governments, themselves or through private contractors, installed systems of piped-water supply and sewerage, while also, goaded by labour organisations, improving housing and working conditions.

In the framework of the STREAM project, a historical-geographical information system was developed based on the map of Count de Ferraris (1771-1777) allowing us to visualise the yearly evolution of mortality ratios.
Principles for the registering of burials were laid down by the Catholic Church in 1614 but it was not before the 1640s that most priests in Flanders and Brabant began to systematically record burials. That is why the number of parishes in the STREAM data set increases overtime.
The maps demonstrate that uncertainty was a fact of life in those days: the risk of death could differ enormously between regions and years.
Video not playing? Watch it on our YouTube-channel!
Causes of excess mortality
Years showing excess mortality are often associated with famine but that in reality seems to have been the exception rather than the rule during the Early Modern period, as in the famine year of 1709. Famine is usually caused by very high grain prices, the result of a failed harvest after a wet summer or cold winter or following obstructions in the imports of grain.
Military activities could also cause destruction or the plundering of harvests. Research has shown, however, that there is no strong link between living standards, as measured by grain prices, and mortality. Years of high prices do not necessarily go hand-in-hand with higher mortality rates and vice versa. There is a simple reason for this. We know from medical research that nutrition does not play a crucial role in the development of many infectious diseases.
The same holds for most of the diseases that determined the mortality pattern in the Early Modern period, such as the plague, typhus, malaria and smallpox. These diseases are so virulent that the nutritional status of a person makes no difference. They do not differentiate between well-fed and malnourished people. The opposite is true for diseases such as dysentery, tuberculosis and cholera; the latter two, in particular, resulting in many victims during the nineteenth century. Unsurprisingly social differences in terms of health were much more outspoken in those days. In the Early Modern period, too, there was social inequality in death but it was conditioned by other factors such as housing and mobility.


Several mortality peaks, especially in the Early Modern period, show a link with wartime, albeit not uniformly. For example, the War of Spanish Succession (1701-13), considered one of the most important, together with the Nine Years’ War (1688-97), as regards duration, army size, and constantly shifting military fronts did not translate into excess mortality.
Naturally, mortality was not only confined to soldiers in wartime but could have serious consequences for civilians too. Armies plundered, destroyed villages and spread diseases and epidemics. A telling example is the passage of the plague in 1667-68 during the War of Devolution. The mortality crisis in 1676-79 has in turn been linked to the spread of dysentery by the troops of Louis the XIV during the Franco-Dutch War (1672-78).
The most serious mortality crises occurred when war, high prices and epidemics coincided. That was the case in 1690 when death rates reached catastrophic proportions in western Europe as a result of the outbreak of epidemic diseases such as typhus and dysentery following a failed harvest and the destructive passage of French troops in the Nine Years’ War.
Lastly, the wars of the French Revolution of the end of the eighteenth century were also responsible for a higher death rate: in addition to the greater number of murders and executions, a dysentery epidemic was responsible for the peak of 1794.
There were also manifest differences between the Duchy of Brabant and the County of Flanders. A crisis could hit one region harder than another or indeed remain entirely untouched by one. As such, at the end of the Eighty Years’ War (1568-48) it was Flanders that was mainly affected. The people in the northwest were subjected to the particularly violent behaviour of the Dutch and Spanish armies.
This was repeated ten years later, this time because of troops in the Franco-Spanish War (1635-59). In 1720 the region was in turn plagued by a serious epidemic of ‘intermittent fevers’, the contemporary term for malaria. This disease already caused higher mortality in the coastal and polder regions outside of peak years due to the many stagnant waters in the region: pools and marshes formed an ideal breeding ground for the type of mosquito that spread malaria, also called ‘marsh fever’ at the time.
Elsewhere in Flanders during the 1720s, many fell victim to typhus, influenza or dysentery. The latter was also the cause of the excess mortality in Brabant in the 1740s and 1780s.

From the medieval plague to COVID-19
The last time the Southern Netherlands were hit by the plague was during the epidemic of 1667-68. Up until that point the disease had descended on the population in successive waves and they were faced with an outbreak every decade or so. It is impossible to tell, however, whether high mortality rates were always caused by the bacteria Yersinia pestis since ‘plague’ was a word that covered a variety of infectious diseases.
For the period preceding the keeping of parish registers, death notices in probate inventories, tax registers and annuities constitute the main sources for gauging the extent of mortality. The most severe outbreak of the plague known as the Black Death devastated the Southern Netherlands from the second half of 1349 onwards with flare-ups until 1351. Europe-wide mortality has been estimated at up to one third of the population.
Some scholars believe that its impact in the Low Countries was not as great because of the better socio-economic conditions here, however, that favourable position has been strongly contested in recent studies.
During the eighteenth century, smallpox took over from the plague as the main cause of death, causing havoc among children in particular. Epidemics at the time tended to be the result of outbreaks of dysentery also called ‘the bloody flux’ because of the bloody diarrhoea accompanying the disease.
A definitive explanation for the disappearance of the plague does not exist, although better rules for quarantine, stronger human immunity, decreasing virulence of the bacterium, or the disappearance of the black rat which spread the disease (probably) via fleas, have been cited as the main reasons.
In contrast, there is no doubt about the reason for the decline in smallpox-related deaths. The discovery of a cowpox vaccine in the late eighteenth century by the English country doctor Jenner, the first vaccine ever, meant the disease could be brought under control in the majority of European countries including Belgium. As a consequence of the Franco-German War, a short but intense flare-up was recorded at the beginning of the 1870s. Today smallpox is the only disease that has been exterminated worldwide.


Clearly, epidemics have always been with us. Many of our ancestors had to learn how to navigate and deal with outbreaks of disease. At first glance, it looks as if history is repeating itself with COVID-19. Many infectious diseases like the plague came from the East and spread via trade routes into Europe.
If you want to use one of the datasets above, do not hesitate to contact queteletcenter@ugent.be.
Or would you like to lend a hand to our new citizen science project www.sosantwerpen.be in which we, together with volunteers, will study the social inequalities in causes-of-death in the city of Antwerp (1820-1946)?
Do you want to know who were the victims of epidemics in the past? Then register via sosantwerpen@ugent.be!
Sources
- UGent, The Quetelet Center, Hisster database, 1804-2019.
- UGent, The Quetelet Center, Stream database, 1640-1796.
Bibliography
- Bruneel, Claude. La mortalité dans les campagnes. Le duché de Brabant aux XVIIe et XVIIIe siècles. Louvain, 1977.
- Devos, Isabelle. Allemaal beestjes. Mortaliteit en morbiditeit in Vlaanderen, 18de-20ste eeuw. Gent, 2006.
- Livi-Bacci, Massimo. Population and Nutrition. An Essay on European Demographic History. Cambridge, 1991.
- Van Gelder, Klaas and Isabelle Devos. “War and Peace in the Time of Malthus. The Demographic Impact of Military Conflicts in Early Modern Flanders, 1650-1800”. Presentation prepared for the European Social Science History Conference, Leiden, March 2020.
- Vermeersch, Joren. 1349. Hoe de Zwarte Dood Vlaanderen en Europa veranderde. Antwerpen, 2019.